Antibiotic Resistance Sequencing - Coming Soon
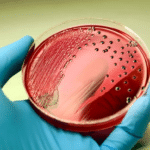
Microbial infections remain one of the most dangerous health complications, worldwide. Understanding the type of microbe that is causing illness is part of the diagnostic tools available to healthcare providers; however, this knowledge only provides list of possible treatments with antibiotics. The presence of antimicrobial resistance (AMR) in the microbes causing an infection may drastically alter the effectiveness of treatments.
Unfortunately, many infections are treated “empirically” using prior experience to guide treatment selection. As expected, this approach may make mistakes, thus delaying more appropriate treatments. When a microbe is identified, healthcare providers may use “directed” therapy that targets a specific organism or set of organisms with known AMR. Targeted use of next generation DNA sequencing can provide unparalleled detection of AMR. This can help healthcare providers decide what not to use and focus on treatments that can work. Doctors may now see all bacteria and survey the AMR with unparalleled accuracy.
With knowledge, treat with confidence.
Information
Introduction
Bacterial culture and drug sensitivity testing have been the “gold standard” in clinical microbiology for more than 70 years. The drawbacks of this approach include the time to culture or grow the microbes, the reliance on secondary biochemical analysis, and the use of secondary drug sensitivity sub-cultures. Less than 2% of all bacterial species can be routinely cultivated; therefore, resulting in many false negative results. These facts create a need for a rapid microbial identification and antibiotic resistance assay that is affordable, accurate, and relevant. Over the last decade syndromic multiplex PCR panels have become increasingly common because of the rapid turn-around-time and affordability. Despite these advantages, these syndromic multiplex PCR panels exhibit a few limitations that include:
- 1. Limited number of detectable microbes that results in a high false negative rate.
- 2. A limited number of antimicrobial resistance genes are detectable.
- 3. Drug treatment confusion when there are two or more identified organisms alongside resistance.
A solution that addresses these limitations is DNA sequencing. Multiple studies, including clinical outcome studies, have been published in the last 5 years in nearly all major clinical specialty disciplines. These studies demonstrate the value and improved clinical outcome as a benefit of molecular and DNA sequencing-based diagnostics.
In 2013, Fry Laboratories was the first commercial laboratory worldwide to offer targeted bacterial (16S) DNA sequencing. This technology has resulted in numerous patents and peer-reviewed publications. This assay, based on a high-quality targeted amplicon approach, is accurate, cost effective, and sample agnostic (it can be used to test blood, urine, CSF, tissue, secretions, bone, and stool). This bacterial DNA sequencing assay is enrolled in both API and CAP proficiency testing programs and has maintained an excellent comparative results track record. A handful of other diagnostic laboratories offer DNA sequencing; however, these laboratories use a non-targeted or “shotgun” sequencing approach that suffers from inefficient sequencing and a more expensive price point. Lastly, this core technology has been independently evaluated by other institutions.

Targeted Resistance to Antibiotics Sequence (TRAXS)
As a result of industrial demand, Fry Laboratories has supplemented our microbial identification system with simultaneous drug resistance detection. Healthcare providers may achieve improved antibiotic treatment insights by using both bacterial and antibiotic resistance gene identification simultaneously. This assay can detect over 900 drug resistance genes and can link them to an organism identified by sequencing based on microbial taxonomy in addition to presenting established treatment information. Together these results are unmatched in microbial detection capability, antibiotic resistance gene detection, and historical treatment information. Currently, no other test or laboratory has this same diagnostic capability. Lastly, we have also developed automation and chemistry advances that make sequencing clinically affordable with acceptable accession to report turnaround time that surpass culture.
Resistance Genes
- AAC – Resistance to aminoglycoside antibiotics.
- ACC – Resistance to beta-lactam antibiotics, but not cephamycin or carbapenem antibiotics.
- ACT – Resistance to beta-lactams antibiotics.
- ANT – Resistance to aminoglycoside antibiotics.
- APH – Resistance to aminoglycoside antibiotics.
- CTX – Resistance to beta-lactam antibiotics.
- dfrA – Resistance to diaminopyrimidine antibiotics.
- dfrB – Resistance to trimethoprim antibiotics.
- ermA/ermB/ermC – Resistance to streptogramin, macrolide, lincosamide antibiotics.
- gyrA – Resistance to quinolone antibiotics.
- IMP – Resistance to cephamycin, penem, carapenem, cephalosporin, penam antibiotics.
- KPC – Resistance to cephalosporin, carbapenem, penam, monobactam antibiotics.
- MCR – Resistance to colistin antibiotics.
- mecA/mecC – Resistance to penam antibiotics.
- MIR – Resistance to monobactam and cephalosporin antibiotics.
- NDM – Resistance to carbapenem, cephalosprin, cephamycin, penam antibiotics.
- OXA – Resistance to cephalosprin, penam, carbapenem antibiotics.
- qnrA/qnrB/qnrC/qnrS – Resistance to fluoroquinolone antibiotics.
- SHV – Resistance to carbapenem, penam, cephalosporin antibiotics.
- sul1/sul2/sul3/sul4 – Resistance to sulfonamide antibiotics.
- TEM – Resistance to beta-lactam antibiotics.
- tetA/tetB/tetD/tetM – Resistance to tetracycline antibiotics.
- vanA/vanB – Resistance to glycopeptide antibiotics.

